The diagnosis of patients with dysphagia can be challenging and often results in their symptoms being attributed to functional dysphagia which is a psychological condition. With testing, typically high-resolution manometry and impedance=pH, careful analysis can prove that the dysphagia is not psychological and therefore treatment options for the patient need to be changed.
Initially, the aim of physiology testing (either impedance-pH monitoring or manometry) is:
- To understand if there is any abnormality in motility or reflux
- To determine whether this/these abnormalities correlate with the symptoms the patient is describing.
- Using this information to advise the clinician on how to treat the patient and manage symptoms.
In this case, a 65-year-old female presented with symptoms of regurgitation, chest pain, belching and dysphagia (feeling of food stuck in the upper oesophagus or gullet).
High Resolution Manometry
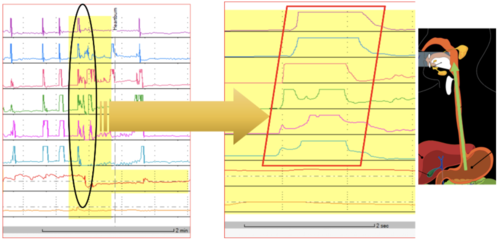
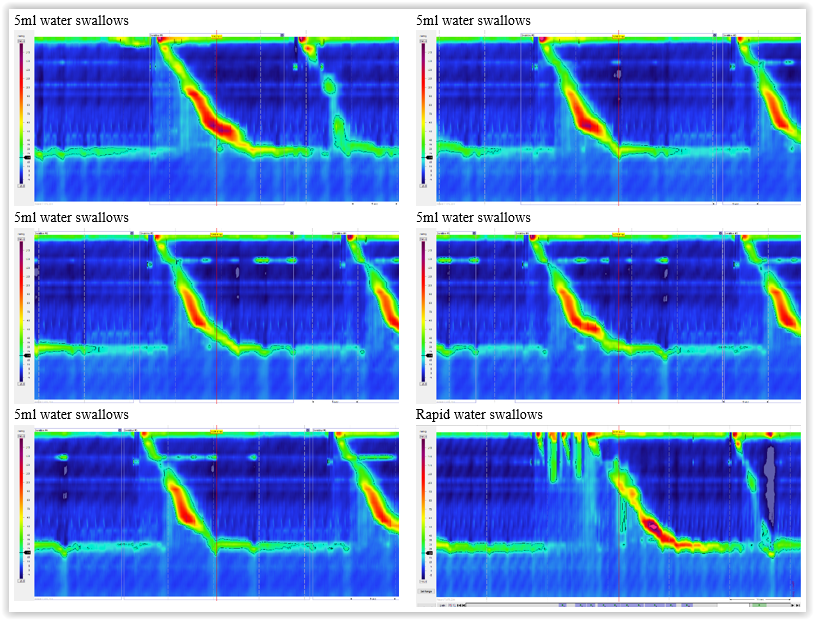
High resolution manometry initially showed fairly normal motility with normal upper oesophageal pressure and relaxation, normal lower oesophageal pressure and relaxation and no hiatus hernia. This would lead to a diagnosis of functional dysphagia. However, when you continue with testing and give provocation tests like multiple water swallows and solid meal swallows the picture changes.
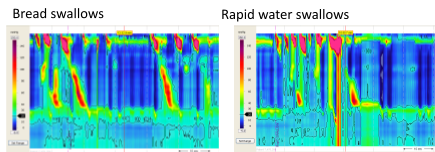
The patient was unable to complete the multiple water swallows, she was then given bread and butter to see what the reaction was. With the first swallow, the patient did not produce any peristaltic contraction and said she was experiencing dysphagia. The next swallow showed good peristalsis and no experience of dysphagia. This pattern continued, with the patient showing good peristalsis and no dysphagia on some occasions and on others no peristalsis and dysphagia on others. When good peristalsis was seen, this cleared any bolus retention. This finding, straightaway changes a diagnosis of psychological dysphagia to one of real dysphagia with abnormal motility corresponding to this symptom. However, this data in itself cannot change the diagnosis as this has to be based on Chicago Classification however it is important and necessary to comment on what was seen. On water swallows, 3/10 peristalsis were weak or with a large gap but the pivotal findings are that the patient perceived dysphagia on solid swallows when there was weak or failed peristalsis.

This finding can exclude functional dysphagia. This is now one step beyond the standard analysis that can help both the clinician and patient.
The cause of the failed peristalsis is not clear, however chronic GORD may contribute to the dysmotility and treating GORD would theoretically improve motility. The next step for the clinician would be to check for GORD with pH-impedance reflux monitoring.
Impedance-pH Reflux Monitoring
Analysis of this data showed that there was pathological reflux in this patient with very high acid exposure at night and borderline normal exposure during the day. Her DeMeester score was high which can indicate the severity of GORD. When looking at symptom correlation, there was a weak association with her symptoms of belching and regurgitation but no association with her chest pain. Further interrogation of the data obtained was carried out to try and ascertain whether her symptoms could be explained by reflux.
Looking at the impedance data and magnifying the reflux episode areas, it was possible to analyse the belching episodes in more detail; as you can see the direction of air.
In this patient, air was seen going downwards and immediately going back up in one second – this is not seen in true gastric belching and is typical of supragastric belching. If this was true gastric belching, you would see both directions going upwards! It is important to ensure that several of these types of episode are seen to enable accurate diagnosis and to make sure this is not an incidental finding.


It was evident that the supragastric belching was triggering reflux. This makes it clear to the clinician that treating the reflux would not treat the belching. The supragastric belching needed to be treated to avoid further daytime reflux that correlated with the patient symptoms in this case. The best treatment for this is oesophageal biofeedback therapy.
Interpretation and Next Steps
This patient showed pathological acid exposure and weakly positive reflux symptom association with belching and regurgitation which led to a diagnosis of supragastric belching. This should be treated by oesophageal biofeedback therapy.
Her daytime acid exposure was marginally normal with the majority of reflux episodes being triggered by supragastric belching. However, as supragastric belching is a voluntary activity of sucking in air and releasing it, it cannot be done during the night which therefore did not account for the patients increased acid exposure at night.
In assessment of the night time reflux, gradual acidification was seen and overall acid exposure was limited towards the end of the night. One explanation for this could be retention of food material or liquid in the oesophagus that gets fermented and becomes acidic – this was not observed in this patient on impedance. During sleep, swallowing is a natural function and can cause relaxation of the lower oesophageal sphincter which results in acid coming up the oesophagus – this was not seen in this case.
There seemed to be a pattern in this patient where with each swallow during sleep time, there was a little bit of acidification which then cleared but it seemed to be happening most of the time. This pattern was not drink induced (the patient waking and drinking in the night) as there was no sign of change of pH in the stomach.
There are two possibilities:
- Acid-only event – the mechanism is not known and why the patient has acidification but the patient needs to be treated as a GORD patient.
- Acidification with each swallow (which theoretically could be an inlet patch – growing gastric mucosa in the oesophagus) may be gradually accumulating and acidifying the oesophagus until around morning.
The night-time reflux is not associated with supragastric belching and therefore, it would be helpful to exclude the presence of an inlet patch in this patient. This can be further investigated by endoscopy.
The possible treatment plan would be, after ruling out the inlet patch, to treat with dual dose proton pump inhibitors (PPI) for at least 8 weeks and if the patient remains symptomatic, to repeat the reflux testing on PPI’s.