A 23 year old lady presented with stomach pain, heartburn, regurgitation, nausea/vomiting and dysphagia.
High resolution manometry and 24-hour pH-impedance investigations were carried out.
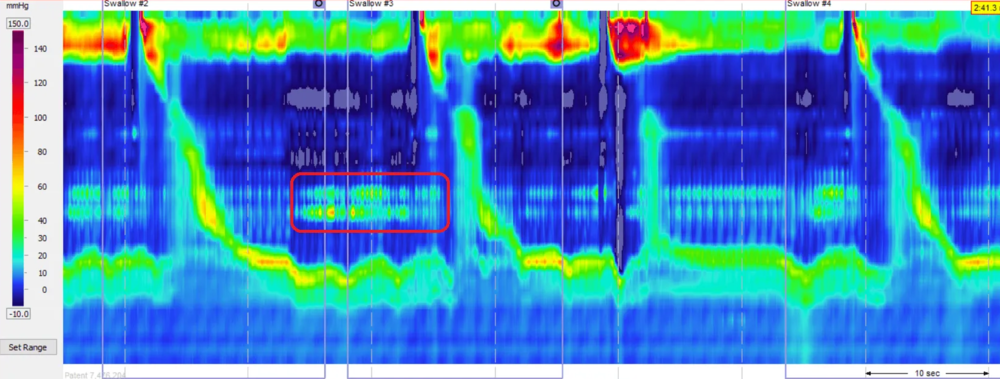
High Resolution Manometry
HRM results showed the following:
- The upper oesophageal sphincter was hypotensive and showed complete relaxation on wet swallows.
- The oesophagus produced weak peristalsis with ≥ 50% swallows with DCI < 450U 9/10 weak/ peristalsis on wet swallows. No typical rumination signs were detected (isolated abdominal contraction-regurgitation/vomit-swallowing during the test).
- The lower esophageal sphincter was normotensive and showed complete relaxation on wet-swallows.
- There was no hiatus hernia.
Based on Chicago classification, the patient was deemed to have ineffective oesophageal motility (IOM).
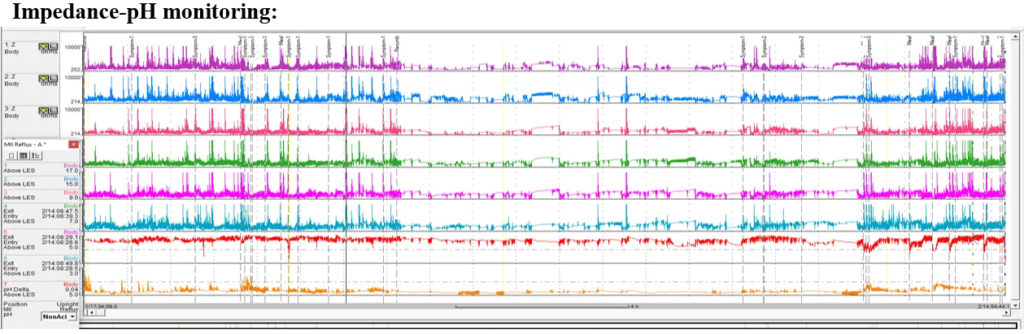
24-hour pH-Impedance Reflux Monitoring Off PPI
The pH-impedance reflux monitoring showed the following results:
- Proximal oesophagus: total 0 episodes, normal <31 (impedance).
- Distal oesophagus: total 0.1%, normal < 4.2%; upright 0.1%, normal <6.3%; supine 0%, normal < 1.2%; DeMeester score: 0.9, normal <14.72; number of reflux events (impedance) total 8, normal <73 (Off PPI).
- Reflux symptom correlations:stomach pain 13 episodes SI = 0%, SAP = 0%; regurgitation 2 episodes, SI = 0%, SAP = 0%; heartburn 2 episodes, SI = 0%, SAP = 0%; positive SI > 50%, positive SAP > 95%.
Interpretation and Next Steps
- The HRM study did not support the presence of rumination syndrome.
- There was a high pressure zone just below the upper esophageal sphincter which could be due to the patient being tense during the investigation or just an incidental finding. However, if there are upper oesophageal symptoms, this should be investigated further, for example an ENT review etc.
- There was no evidence of pathological acid/non-acid reflux.
- There was no positive reflux symptom association for stomach pain, regurgitation and heartburn
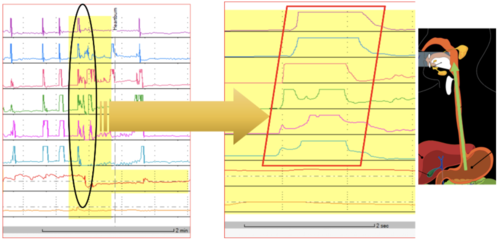
- There was very little reflux detection in this study and no evidence to support rumination syndrome of other behaviour GI phenomena such as supragastric belching or regular regurgitation-swallowing episodes in this patient.
The most beautiful part of this study that can help the clinician in developing a proper treatment plan is that the stomach pain was reported 13 times and at no point was this preceded by any type of reflux (acid or non-acid). The same was true with regards to heartburn and regurgitation although fewer symptoms were reported. This picture is compatible with a diagnosis of a Functional GI Disorder – other potential causes of patient symptoms must be excluded before making this diagnosis. This term means that for the time being, that the medical knowledge has hit a wall! However, we know that in functional states, trials of SSRIs, such as amitriptyline or pregabalin can be helpful. The patient must be made aware that it can take up to 8 weeks to decide on the effectiveness of the treatment before moving to another medication.
During this study, the patient reported that they did experience around 60% of their usual symptoms. This test could be repeated if the patient believes they did not have their usual amount of symptoms. In this case, we have enough information, as per the above explanation to come to a solid conclusion.